As of 28 July 2024, a total of 14,250 cases of mpox (2,745 confirmed; 11,505 suspected) and 456 deaths have been recorded in 10 African countries, including Burundi, Cameroon, Central African Republic, Congo-Brazzaville, Democratic Republic of Congo (DRC), Ghana, Liberia, Nigeria, Rwanda and South Africa.
The DRC outbreak, ongoing since 2022, accounts for more than 90% of the reported cases of severe mpox clade 1b. This year, the DRC identified 13,791 cases, with children under 15 accounting for 68% of cases and 85% of deaths.
Four countries – Burundi, Kenya, Rwanda and Uganda – previously unaffected by mpox, have reported cases since mid-July 2024 (at least 50 confirmed cases, with clade 1b now confirmed in Kenya, Rwanda and Uganda).
There is a vaccine that is effective against both clades, but it is not widely available. The resources to contain and avoid this unfolding crisis exist but must be brought to bear to contain the outbreak with the greatest urgency possible.
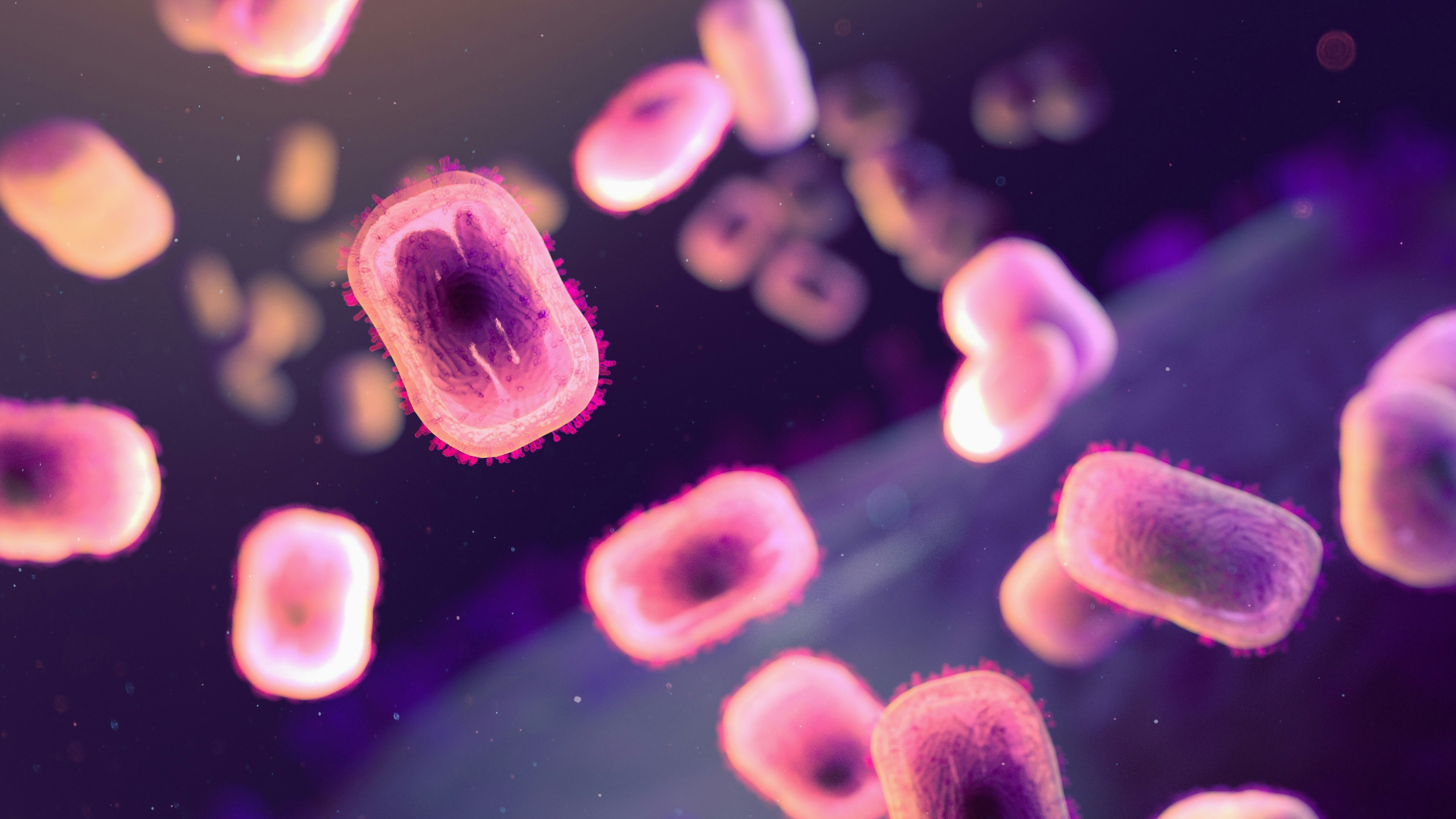
This zoonotic virus, endemic to the forested regions of east, central and west Africa, has shown increased human-to-human transmission, including by way of sexual transmission, which deviates from the historically zoonotic (animal) nature of the disease.
Kenya’s Ministry of Health confirmed an outbreak of mpox clade 1b on 29 July 2024, originating from a traveller moving through Uganda and Rwanda. The development underscored the urgent need for enhanced public health measures across east Africa, as the high mobility of populations through key transport corridors poses a significant risk for regional transmission.
The urgency to address the outbreak is made keener by the fact that some infected individuals may be contagious before they develop symptoms. With the DRC reporting rising cases, and other countries experiencing mpox for the first time, the situation calls for urgent coordinated efforts to prevent a broader health crisis.
There is a great need to strengthen the healthcare systems of many African countries. The DRC has faced significant challenges in its healthcare infrastructure due to historical under-investment. This has resulted in limitations in diagnostic capabilities, technology, and workforce expertise, which have impacted the response to the outbreak. The province of South Kivu, particularly the mining town of Kamituga, has been severely affected, with the situation further complicated by socioeconomic factors.
As the outbreak has spread to east Africa and beyond, the region’s healthcare systems, which are continually striving to improve their resilience and capacity, are experiencing considerable pressure.
Collaborative efforts at both regional and continental levels are essential to bolster these systems and effectively manage the current health challenges.
There is also a need for greater cross-border surveillance, detection, prevention and treatment. The Institutional Framework for Cross-Border Integrated Disease Surveillance and Response (IDSR) in the east Africa region, published in 2019, recommended the establishment of smaller surveillance units to capture the increasing number of infectious diseases spread from animals to humans.
The framework emphasised the importance of establishing cross-border disease surveillance zones and response committees to coordinate and implement interventions. It outlined the need for integrated disease surveillance systems, with mechanisms for sharing epidemiological information and conducting joint planning for epidemic preparedness and response.
The East African Community’s Institutional Framework highlights the importance of strengthening the network of medical reference laboratories and establishing rapid response mechanisms to protect the region from health security threats. Enhancing these capacities will enable quicker detection and response to outbreaks like mpox, minimising their impact on health and socio-economic activities. Increasing access to safe, efficacious, and affordable medicines and vaccines is a key priority.
The Institutional Framework calls for establishing a regional pooled bulk procurement mechanism and strengthening national medicines regulatory authorities. Ensuring equitable access to vaccines, such as those for mpox, is critical for controlling outbreaks and protecting public health. However, when it came to funding the framework, it had a budget of only $225,000.
The Africa CDC recognises the critical need to address health challenges and emergencies effectively across the continent. In response to these challenges, it has developed a continental strategic framework to strengthen cross-border surveillance, coordination, and information sharing among African Union (AU) member states.
This framework is designed to address the increasing frequency and magnitude of cross-border public health threats in Africa, driven by population movements, globalisation, and human, animal, and environmental interactions within ecosystems.
By focusing on points of entry such as airports, seaports, and land borders, the framework aims to bolster the continent’s preparedness and response to health emergencies, contributing to the overall resilience and robustness of public health systems across Africa.
While African countries strive to manage the outbreak, international cooperation and support are critical. The WHO and Africa CDC provide important financial and technical assistance for epidemic and pandemic response, yet the disparity in access to resources between high-income and low-income countries remains stark. Both agencies have now acted.
The AU announced that it had approved $10.4-million from Covid funds for the mpox response, while WHO chief Tedros Ghebreyesus called for more funding to support a comprehensive response, including for diagnostics, therapeutics and vaccines.
Ghebreyesus also called for an emergency committee meeting to determine whether the outbreak constitutes a public health emergency of international concern, and on Friday, 9 August, the WHO issued an invitation for manufacturers of mpox vaccines to submit an expression of interest for emergency use listing.
Meanwhile, Africa CDC plans to meet with the AU next week to seek their backing for declaring a public health emergency of continental concern. This would be the first such declaration in the agency’s history.
Many countries, including the United States, have committed assistance.
The US Center for Disease Control issued an alert to healthcare providers, advising them to consider mpox as a possible diagnosis for patients. As part of $424-million in humanitarian assistance to the DRC, USAID announced $10-million in health assistance for interventions in response to the current outbreak. Additionally, USAID is donating 50,000 mpox vaccine to the DRC.
In related news, the US’s Biomedical Advanced Research and Development Authority announced nearly $157-million for Bavarian Nordic to “partly replenish” US government stocks of the Jynneos smallpox/mpox vaccine.
As mpox has spread to the Global North, vaccines have become an unmet global need.
In addition to illness and loss of life, there will be financial consequences to this emerging threat. Africa Risk Capacity (ARC), a specialised agency of the African Union, has developed a sovereign parametric risk insurance product aimed at providing rapid financial support to countries during outbreaks and epidemics.
This initiative draws from ARC’s successful experience in climate risk financing, where it has helped countries like Zimbabwe and Zambia receive payouts for climate-related disasters such as droughts.
However, ARC’s current insurance product for outbreaks is focused on a limited scope of pathogens, specifically Ebola virus disease, Marburg virus disease, Lassa fever and meningococcal meningitis. These pathogens were chosen due to their significant epidemic potential and historical impact on the continent. Given this focus, it is unlikely that mpox will qualify for ARC support under the current framework.
The exclusion of mpox from ARC’s coverage highlights the need for a broader approach to pandemic insurance that can address a wider range of infectious diseases.
While ARC’s efforts are commendable, expanding the scope to include emerging threats like mpox could enhance Africa’s preparedness and resilience against diverse health challenges. Development banks must put more skin in the game.
By investing in preparedness and response in a collaborative framework, Africa can better protect its populations from emerging infectious diseases.
It is imperative that countries act swiftly to prevent the further spread of mpox and safeguard the health and well-being of those in Africa and beyond. Immediate actions should include convening a regional summit to strategise on resource mobilisation and sharing of best practices.
The lessons learnt from previous health crises, such as the Ebola and Covid pandemics, emphasise the need for proactive and coordinated cross-border responses.
A key lesson is that the highest offices in the land must ensure that the whole of government pays attention, which requires that presidents and prime ministers lead from the front.
The WHO and Africa CDC are technical support agencies, but it is up to individual governments to act and commit resources from their national budgets, as challenging as that is, given current fiscal constraints. Saving lives and livelihoods matter. DM
Peter Babigumira Ahabwe is the co-chair of the Global South Workstream of the Global Health Security Agenda Action Package on Biosafety and Biosecurity. Andrea Uhlig is Research Associate at the Pandemic Center, Brown University School of Public Health. Lawrence R Stanberry is Professor of Pediatrics at Columbia University’s Vagelos College of Physicians and Surgeons. Wilmot James is a Professor of Practice and Senior Advisor to the Pandemic Center, School of Public Health at Brown University.
This article is more than a year old
Africa
Mpox outbreak in the DRC – a call for an urgent collaborative continental response
The urgency to address the outbreak is made keener by the fact that some infected individuals may be contagious before they develop symptoms.